History
Incorporation
Manitoba Bone and Joint Health Inc. (MBJH) is a registered corporation (2005) under Manitoba’s Corporations Act to foster provincial and federal coordination of bone and joint musculoskeletal (MSK) care. Pursuit of coordinated global bone and joint care was initiated through the International Bone and Joint Decade in 2000, Next decade this was rebranded the Global Alliance for Musculoskeletal Health. Alberta Bone and Joint Health (2003), Bone and Joint Canada (2007), and the Bone and Joint Health Network of Ontario (2010) are active MSK umbrella organizations. The National Health Service in Britain introduced The Musculoskeletal Services Framework in 2006 to coordinate bone and joint care as “A Joint Responsibility: Doing it Differently”. In addition , in Alberta which has reduced to a single provincial health department, a strategic clinical network (Alberta Bone and Joint SCN) now provides provincial oversight to MSK care . Refer to the Links page to access these networks. The federal government of Canada in 2012 directed the provinces to increase their role in coordinating and providing health care. We consider this a formal federal request for a province-wide MSK framework in Manitoba.
Demographic Problems and Solutions
Problem of access to care: The aging boomer generation brings a greater demand for bone and joint care. First Nations MSK health calls for better coordination. Growing provincial and federal deficits hamper application of costly new technologies and increasingly expensive care for an aging population. Low income citizens suffer inferior health outcomes compared to the more affluent.
Solutions: Preventive strategies, coordination of hospital, community and longer-term care require ongoing review and development of provincial strategies for bone and joint care.
Problem of deploying orthopedic surgeon workforce: Only a decade ago there was a perceived national shortage of orthopaedic surgeons. Now there is surgeon oversupply relative to available operating rooms, equipment, beds, and affiliated human resource, but restricted patient access and prolonged wait times persists.
Solutions: Better provincial coordination to match resources and needs with changing technology and economics. This requires a provincial focus on bone and joint care in its entirety. Including private sector service participation (publicly administered according to the Canada Health Act) reduces the tendency to underperformance of undirected monopolistic government control of services .
Problem of competition for resources: Within orthopedics, greater funding of hip and knee replacement activity displaces support relative to other bone and joint disciplines, impeding care for those suffering with foot and ankle, hand and wrist, shoulder and other MSK problems. In global health care budgets, orthopedics and other MSK disciplines compete with other health care segments for limited resources. Health care regions compete with one another for a bigger share of resources, and offload or abandon what they do not budget for. Debt burdens grow to meet existing and expected obligations.
Solutions: Provincial frameworks exist to encompass, prioritize, innovate, share, collaborate and expand. They are positioned provincially to relate also to federal participation in health care.
Problem of fear in Canada of a two-tiered system of care leaving out the poor and disadvantaged: The private sector is thoroughly ingrained in the system already in capital construction, charitable foundations, human resources, consulting services, equipment and devices, support services, and the direct provision of health services not insured under provincial plans. Third party payers (Workers Compensation, federal government, provincial automobile insurance, DND, RCMP, and private insurance companies) all provide services and funding to the system.
Solutions: If provincial health care is organized by disease groupings or body systems, such as Cancer Care and Bone and Joint Care, private care is an addition and option , rather than segregator and depleter of resources. This expands access, while remaining publicly administered.
Background to a Patient Centred Framework to Systematize Bone and Joint (MSK) Care Provincially
A MSK framework to systematize bone and joint care overviews orthopedic subspecialization, delegation of health care responsibility to regional health authorities, consolidation of surgical services to fewer locations, through the patient centred model of health care.
Orthopedic Subspecialization in Manitoba
In 1990, specialization in orthopedics was in its early stages. There were adult and child (pediatric) orthopedics. In earlier decades, some surgeons and hospitals were known for special interest in such areas as spine, trauma, and hand surgery, but the majority of surgeons and hospitals pursued a general, broad scope of orthopaedic services.
Twenty years later, most young orthopedic surgeons outside of small centres are subspecialized into not more than two areas of orthopedics, and most older general orthopedic surgeons have progressively reduced their range of practice.
A current list of orthopedic subspecialties includes: hip & knee replacement, shoulder & elbow replacement, hand & wrist, foot & ankle, sports medicine & surgery, spine surgery, and trauma surgery. There has been further subspecialization within pediatric orthopedics.
Technological advances and a growing range and complexity of orthopedic procedures have led to subspecialization of orthopaedic care, contributing to fragmentation of MSK care.
Regionalization of Health Care in Manitoba
By the Regional Health Authorities act of 1996, legislation was introduced to enable the Ministry of Health to delegate health care delivery to eleven regions (RHA’s) in Manitoba.This was done without an orchestrating template for all diseases other than Cancer Care.
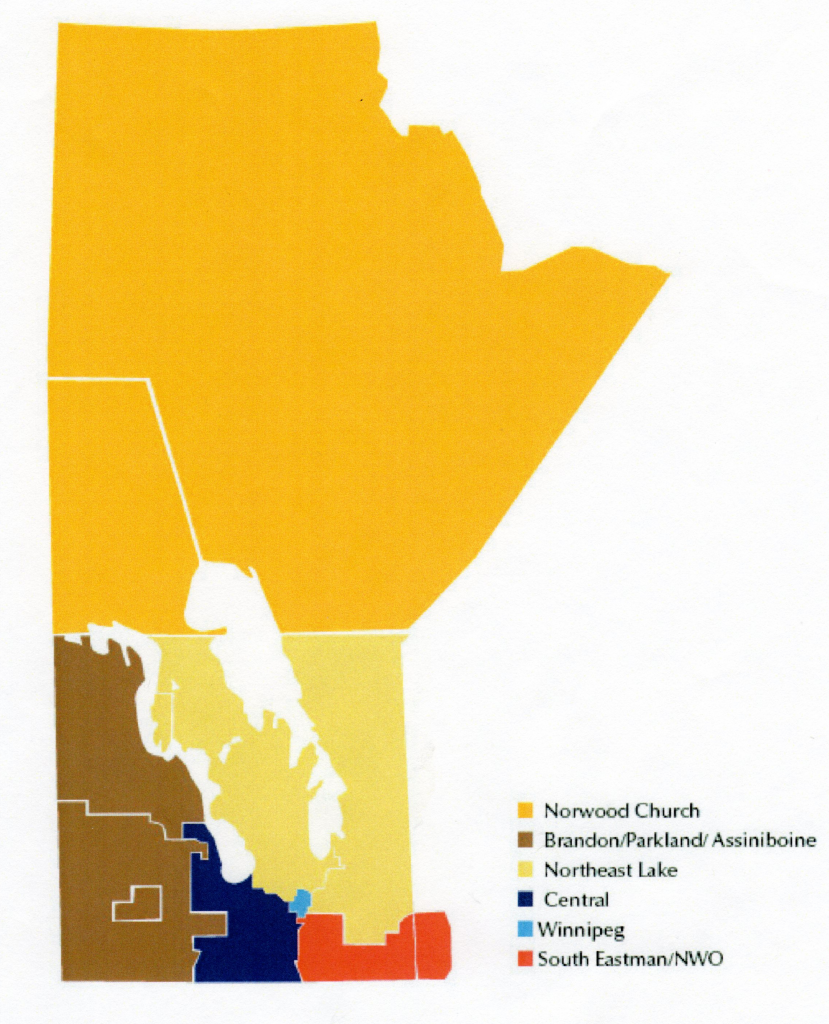
Most orthopedic surgery was concentrated in the Winnipeg region. Brandon had a long history of orthopedic surgery, and after Winkler and Morden combined their hospitals to create the Boundary Trails Health Centre, orthopedics joined the general surgeon already there. MBJH in 2007 proposed that orthopedics in the eleven RHAs be condensed down to six regions for easier coordination of provincial Bone and Joint Care. The map proposed for regionalized MSK organization is shown (Fig 1)
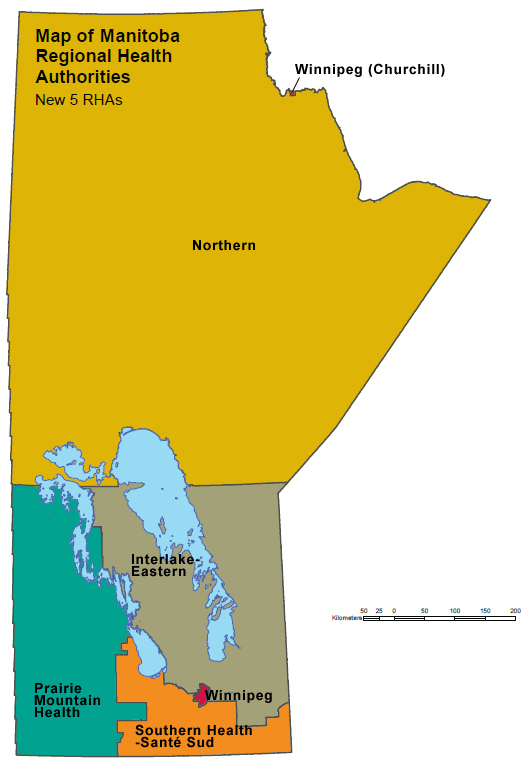
This proposal was not adopted, but in 2012, for administrative purposes, Manitoba reduced the total number of RHAs to five (Fig 2), resulting in a map quite similar to our 2007 MSK proposal. Although the Manitoba Health 2012 consolidation was to reduce administrative costs, an additional benefit is to similarly reduce the number of Bone and Joint groups needed to create an umbrella provincial system of Bone and Joint care.
Consolidation of Surgical Services in Manitoba
Cardiac surgical care has been consolidated from two major Winnipeg hospitals to one, most revision hip and knee replacement surgery from four sites down to one, general surgery emergencies from 6 hospitals to three, and orthopaedic emergency surgical care from six hospitals to three. Morden and Winkler consolidated two rural general hospitals, including surgical services, to the single regional Boundary Trails Health Centre. This process may continue even further provincially, to put combined expertise and resources together to provide more services of a narrower range in specialized hospitals, reducing the number of general hospitals.
Implications for Provincial Organization of Health Care by Systems
The processes of subspecialization, regionalization, and consolidation result in a need for a provincial plan to determine how much bone and joint activity should be provided in each region, what level of complexity is possible/desirable and how much of this activity should be available in various region, to reduce the clamour of uncoordinated competing, overlapping, proposals and demands. A provincial MSK enables including a greater role for private care that does not detract from the public component. In the absence of the MSK framework, the Winnipeg Health region by default directs provincial MSK health care activity. The legislated responsibility for this is removed from the health ministry. The result is a loss of responsibility and accountability.
Major Health Issues in Manitoba Related to Bone and Joint Care
Diabetes contributes to severe bone and joint problems including septic arthritis, neuropathic joint destruction, and amputations. As diabetes increases, so may the incidence and losses from these MSK problems. Internet teleconferencing is one way to expand services and reduce costs.
Osteoporosis fracture patients seen in emergency departments and clinics, are at higher risk for refractor. An MSK framework can combine resources to reduce recurrences.
Aging and geriatric patients lose independence and require more long term care related to progressive decline in bone and joint function. Many disciplines in health care are involved can be included through the MSK framework as an example of preventive care.
Level of income is the primary determinant of health in a population, so both raising productive income for the poor, and better use of available income should both improve the health of the population. MSK health is critical for an ability to earn income for much of the population.
Other topics to consider from a provincial, multidisciplinary approach to Bone and Joint Health include:
- Arthritis and maintenance of function
- MSK education among MSK related disciplines
- Weight reduction exercise programmes, avoidance of MSK injury, and associated reduction of surgical demand
- Bone and joint injuries in the workplace in the presence of pre-existing MSK disease remains a management challenge for Worker’s Compensation Board and injured workers.